1. Oral Medication before Events
Warfarin was administered to 49 patients (100%), aspirin to 48 (98%), ACE-I to 16 (33%), ARB to 30 (61%), β blocker to 15 (31%), aldosterone blocker to 11 (22%), and bosentan to 5 (10%).
2. Infarction Cases (Table 1)
Table 1 Characteristics of patients with cerebral infarction| Case | Age of onset (years) | Years after Fontan procedure (years) | Surgical procedure | Diagnosis | Risk factors for thromboembolism | Drugs | PT-INR |
|---|
| 1 | 35 | 18 | Ex-TCPC (TCPC conversion) | TA1b | Pulmonary arterio-venous fistula | W+A interrupted | 1.28 |
| 2 | 26 | 18 | Lt-TCPC | DORV | Pulmonary blind pouch | W | 2.13 |
| 3 | 15 | 5 | Ex-TCPC | Asplenia | Artificial valve | W+A | 1.80 |
| A, aspirin; DORV, double outlet right ventricle; Ex, extra-cardiac conduit; Lt, lateral tunnel; TCPC, total cavo-pulmonary connection; TA, tricuspid atresia; W: warfarin. |
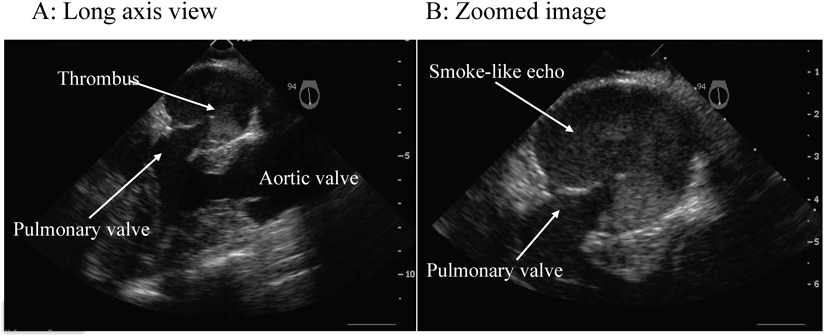
Cerebral infarction was observed in three of 49 patients (6%). The age at onset in these three patients was 35, 26, and 15 years, and on routine examination before the onset, thrombi were not detected. In case 1 with underlying pulmonary arteriovenous fistula, aspirin was discontinued because of severe hypermenorrhea and warfarin was also subsequently withdrawn, during which time cerebral infarction occurred. At the time of the onset of cerebral infarction, PT-INR was 1.28 and the D-dimer level was 0.13. In case 2, who responded to warfarin monotherapy with a PT-INR of 2.13, paralysis developed, and TTE and transesophageal echography (TEE) revealed a thrombus in the blind intracardiac pouch stump with a smoke-like echo (Fig. 1). Following hospitalization, heparin and brain-preservation therapy was initiated, and with concurrent aspirin, the subject recovered from the cerebral infarction. However, during follow-up, renal infarction occurred; therefore, after increasing the warfarin dose, surgery was performed for pulmonary atresia. Case 3 was a patient who had undergone atrioventricular valve replacement, and while receiving oral warfarin and aspirin therapy, paralysis and anarthria occurred when PT-INR was low at 1.80. TEE revealed intra-arterial mural thrombus with a smoke-like echo.
Fortunately, all patients were admitted to the Department of Neurology, where the symptoms were alleviated with thrombolytic therapy and without any sequelae.
3. Hemorrhage Cases
No cases of cerebral hemorrhage were observed.
Gastrointestinal bleeding was observed in three patients (Table 2).
Table 2 Characteristics of patients with gastrointestinal hemorrhage| Case | Age (years) | Chief complaint | PT-INR | Pre Hb | Post Hb | Aspirin | H. pylori | Blood transfusion | Emergency endoscopy |
|---|
| 1-① | 6 | Common cold, fever | 1.77 | 10.7 | 5.4 | 1.8 mg/kg/day | Not examined | + | Not done |
| 1-② | 7 | Pale face | 1.66 | 10.5 | 6.1 | 1 mg/kg/day | Not examined | + | Not done |
| 1-③ | 8 | Fatigue | 1.82 | 13.7 | 8.9 | 1 mg/kg/day | Positive | − | Not done |
| 1-④ | 15 | Pallor | 3.50 | 15.0 | 9.4 | Enteric-coated aspirin 100 mg/alternate-day | Negative (after pylorus eradication) | + | Bleeding ulcer |
| 2 | 19 | Fatigue | 2.74 | 15.8 | 7.7 | Enteric-coated aspirin 100 mg/alternate-day | Negative | + | Bleeding ulcer |
| 3 | 9 | Abdominal pain | 2.23 | 12.7 | 4.7 | 1.25 mg/kg/day | Negative | + | Bleeding ulcer |
| 1-①–④ denote four episodes in the same patient. |
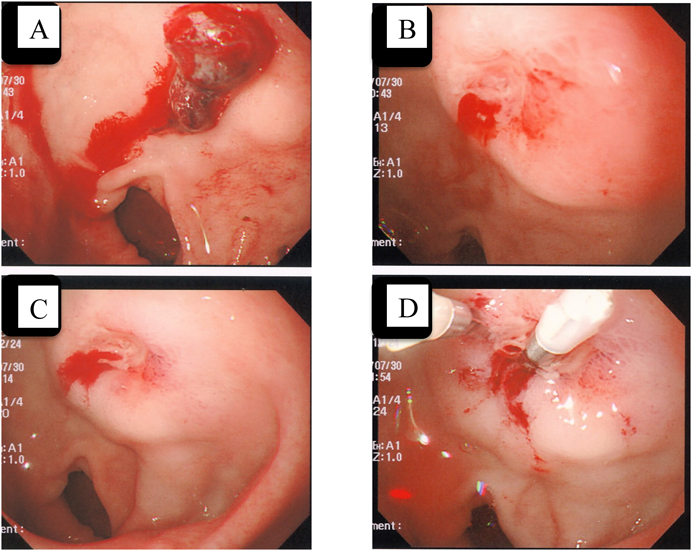
Three patients exhibited a total of six events of gastrointestinal bleeding. Only one of these three patients complained of abdominal pain. Five hemorrhagic events required emergency transfusion, and all patients were receiving oral warfarin and aspirin therapy. Events 1–4 occurred in the same patient (asplenia). The site of the hemorrhage could not be diagnosed using lower gastrointestinal contrast-enhanced endoscopy and Meckel diverticulum scintigraphy performed at the time of events 1 and 2 and using endoscopy performed several days later. At the time of event 3, urine was clearly positive for Helicobacter pylori antigens, and bacterial elimination was unsuccessful. Therefore, aspirin was discontinued because of the risk of ulceration. When the patient was 13 years old, H. pylori was successfully eliminated with the combined use of metronidazole, and alternate-day administration of enteric-coated aspirin tablets was recommenced. However, at 15 years of age, the subject underwent atrioventricular valve replacement, and ulceration recurred 2 months later (case 1, event 4). At this point, emergency endoscopy following blood transfusion revealed the adhesion of a blood clot to the posterior wall of the duodenal bulb, below which a superficial ulceration of approximately 3 mm and an exposed vessel with arterial bleeding were confirmed. As bleeding could not be completely stopped with a hypertonic saline injection, hemostasis was implemented with clipping (Fig. 2). Case 2 was a 19-year-old male (PA-IVS with sinusoidal communication, old myocardial infarction, and occlusion of the left anterior descending coronary artery) who noticed blackish feces several days earlier with no abdominal pain. As examination revealed the subject to be in a pre-shock state and pale, he was hospitalized. Case 3 was a 9-year-old boy (TAIIc and CoA) who was conscious, oriented, and alert and the only patient to complain of abdominal pain, for which he consulted a local pediatrician. However, abdominal echography revealed no abnormality, and constipation was diagnosed. An enema was given, and his condition was monitored. He went into a state of pre-shock 5 days later. Despite instructing his mother to pay frequent attention to whether any blackish feces appeared, she did not observe any.
Apart from case 1, event 3, for all patients, emergency transfusion was required, and after discontinuing warfarin and aspirin, menatetrenone was administered and the combined use of proton-pump inhibitors (PPI) was initiated. Thereafter, once in a stable condition, warfarin alone was recommenced in all patients while continuing PPI therapy. However, only in case 2, coronary sequelae were observed. Thus, on the following day, enteric-coated aspirin tablets were recommenced on alternate days.
Pulmonary Hemorrhage Occurred in Three Patients
A 27-year-old male with asplenia and a history of atriopulmonary connection surgery died of critical pulmonary hemorrhage 14 years after undergoing the Fontan procedure. As the patient had long exhibited bloody sputum, cardiac catheterization was recommended. However, following previous cardiac catheterization contrast-enhanced imaging, macroscopic hematuria was observed, but the patient had refused to undergo cardiac catheterization for 10 years. During oral warfarin and aspirin therapy, although PT-INR at hospitalization was relatively low at 1.48, massive bleeding occurred suddenly and the patient’s life could not be saved. The presence or absence of abnormal collateral vessels was unclear as they were not investigated on computed tomography (CT) or echography, and consent was not obtained for pathologic autopsy.
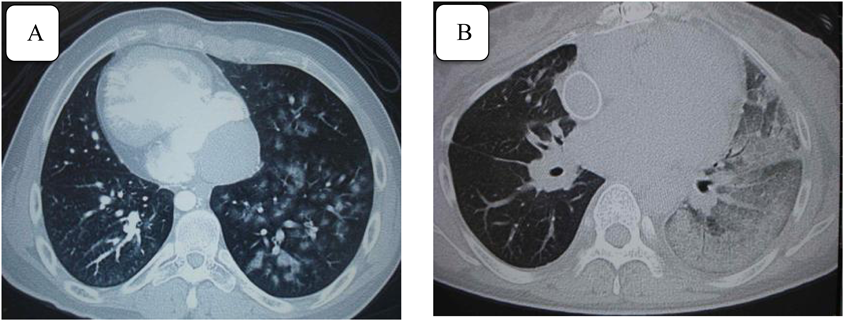
A 19-year-old male with MA and a history of atrioventricular valve replacement surgery suffered from diffuse alveolar hemorrhage 16 years after undergoing the Fontan procedure (Fig. 3-A). Even after coil embolization of the collateral vessels, hemoptysis repeatedly occurred, which resolved upon the discontinuation of aspirin. Therefore, despite the artificial valve, the warfarin dosage had to be temporarily reduced. The Department of Respiratory Medicine was consulted, and continuous low-dose clarithromycin therapy alleviated the hemoptysis attacks.
The aforementioned 38-year-old female with a history of cerebral infarction (TAIb) was being treated with warfarin alone. However, during a routine health check-up 3 years after the cerebral infarction, an infiltrative shadow was identified in the left lung, and pneumonia was initially suspected. However, the shadow gradually grew and pulmonary hemorrhage was diagnosed by CT (Fig. 3-B). PT-INR at diagnosis was 2.29. Therefore, the warfarin dosage was temporarily reduced, and the hemorrhage resolved without any recurrence of cerebral infarction.
Other Cases (Some Patients with Multiple Symptoms)
Severe subcutaneous bleeding occurred in four patients. Two patients had frequent nose bleeds, severe hypermenorrhea, and repeated epigastric pain. One patient had macroscopic hematuria, ovarian bleeding, aspirin-induced rash, and hepatopathy.
All patients were successfully treated by discontinuation of aspirin, reduction of warfarin dose, and administration of hemostatic drugs. Furthermore, some patients with cuts and contusions required some time for hemostasis to occur but could be treated by covering/sealing with an alginate dressing and without changing the oral therapy.
In patients with a mean PT-INR of 1.9±0.5 (1.47–2.31) at the time of a hemorrhagic event and who were receiving warfarin combined with aspirin, the hemorrhagic event occurred irrespective of PT-INR. A high PT-INR did not imply bleeding, and routine blood sampling conducted 1 week after vomiting and diarrhea revealed that although some patients showed a temporarily elevated PT-INR of up to 10.5, fortunately no hemorrhagic event occurred.
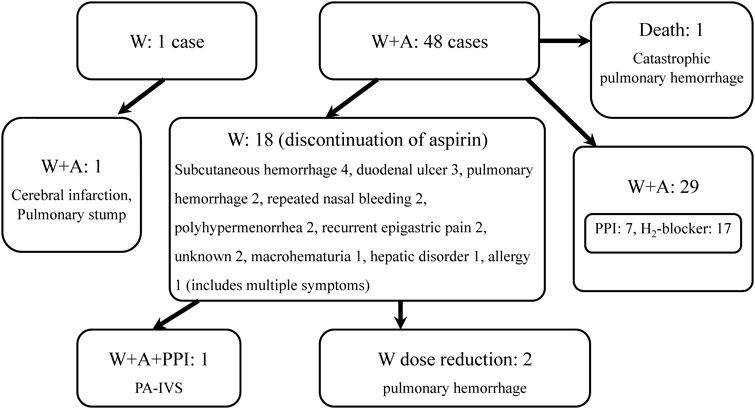
4. Changes in Medication Following an Event (Fig. 4)
In patients with a residual blind intracardiac pouch pulmonary artery stump who suffered cerebral infarction, warfarin and aspirin therapy was initiated. In 18 patients, including those with pulmonary hemorrhage and gastrointestinal bleeding, aspirin was discontinued and warfarin monotherapy was started. Two patients with pulmonary hemorrhage required a temporary warfarin dose reduction, and aspirin was recommenced only for the PA-IVS patient with a coronary lesion upon administration of PPI. Furthermore, in the 29 patients receiving both agents, prophylactic PPI or H2 blockers were initiated regardless of the presence or absence of ulceration. Following the initiation of antiulcer agents, no patient suffered from gastrointestinal bleeding.
Among the adult patients who undergo the Fontan procedure, approximately 17% (one in every six patients) have silent pulmonary emboli, which have not been observed in patients receiving warfarin therapy.3) At the same time, if silent emboli gradually increase pulmonary vascular resistance, then anticoagulant therapy might improve the long-term functioning of Fontan circulation, thereby improving survival. When the blood flow velocity becomes slow, red blood cells form a rouleaux and increase shear stress, thereby causing the von Willebrand factor (vWF) to change and cause increased thrombotic tendency.2) However, in normal laminar flow, it is unclear how vascular endothelial cells with antithrombotic function change in the Fontan circulation and how polycytemia and a congested liver affect liver-derived clotting factors.
According to a report on adult atrial fibrillation, compared to the clopidogrel and aspirin combination therapy group, the warfarin monotherapy group exhibited a greater event-prevention effect.6) Although fibrin thrombi anticoagulant therapy is considered to be superior to the antiplatelet therapy, for the treatment of Fontan venous thrombosis, warfarin and aspirin are comparable.
According to the 2011 report from the Fontan Anticoagulation Study Group by Monagle et al.,4) a 2-year multicenter prospective controlled study of warfarin and aspirin for the primary prevention of TE following the Fontan procedure revealed no difference between the two groups, and the preventive effect itself in the two groups was therefore considered inadequate. Thus, it is concluded that to prevent TE in the long-term, future studies should examine unlimited factor Xa inhibitors, novel oral anticoagulants (NOAC) used in combination with warfarin and aspirin, and the intensification of antiplatelet agents. In future clinical trials, to determine whether microvascular TE has an adverse effect on pulmonary and systemic circulations, the need for regular TEE has been proposed. In the secondary analysis of the same trial, McCrindle et al.5) reported that at 2.5 years following surgery, 31% of the patients exhibited thrombosis, with no difference observed between the warfarin and aspirin and the warfarin-poor control groups (PT-INR<2.0); in contrast, thrombosis was more common. However, on the other hand, as all thrombi were venous, it is concluded that NOAC must be examined in the future.
Manlhiot et al.7) reported that TE prevention is needed during the period following the initial palliative surgery in patients with a single ventricle and Glenn’s operation, as well as the Fontan procedure. They also reported that enoxaparin and low-molecular-weight heparin exhibit a preventive effect following the initial palliative surgery and the Glenn operation, whereas following the Fontan procedure, the preventive effect in the warfarin group was superior to that in the aspirin and nontreated groups, with no difference in the hemorrhagic complications.
In contrast, Uno et al.8) measured thrombin–antithrombin-3 complex and α2-plasmin inhibitor–plasmin complex levels in a 16-year-old child following the Fontan procedure. Because both levels had normalized at 12 months postoperatively, they proposed administering warfarin for 1 year postoperatively, then subsequently changing to antiplatelet therapy. Ohuchi et al.9) examined patients who were administered warfarin in combination with aspirin following the Fontan procedure and reported that hemorrhagic complications arose early and that TE commonly developed within 6 months and 15 years postoperatively. Thus, in low-risk patients, warfarin should be discontinued at 1 year after the Fontan procedure to reduce hemorrhagic complications. However, in 7% of the patients, warfarin was recommenced, and it has been indicated that as PT-INR was not examined, it is difficult to standardize the anticoagulant therapy.
According to Hallas et al.,10) in recent years, adults with atrial fibrillation are increasingly being administered several antiplatelet agents and anticoagulants in combination, and in a study of gastrointestinal bleeding, it was reported that when the adjusted odd ratios for aspirin monotherapy and warfarin monotherapy were 1.8, respectively, the corresponding odds ratios for combined use were 5.3. Thus, the need for ulcer prevention in combination therapy is considered more and more important. Furthermore, in the Hokusai-VTE trial11) for the treatment of adult venous thrombosis and the inhibition of recurrence, compared to warfarin, edoxaban, a factor Xa inhibitor, showed noninferiority in terms of effectiveness and superiority in terms of safety, such as for bleeding.
In young patients with few thrombi, it originally was difficult to determine whether microvascular TE leads to Fontan circulatory insufficiency. In the past, it was said that following the Fontan procedure, elevated CVP, low output, and hepatopathy reduce various anticoagulation factors. However, Odegard et al.12) reported that in children with HLHS, the risks of thrombosis include markedly elevated factor VIII levels and reduced protein C levels. In contrast, Tomkiewicz-Pajak et al.13) reported that in adults undergoing the Fontan procedure, all coagulation factors, including factor VIII, were low but at the lower limit of normal. Although low levels of coagulation factors are characteristic, bleeding is not common, and elevated prothrombin fragment F1+2, which is a marker of thrombin generation, with an elevated tissue factor pathway inhibitor gives rise to the hypothesis that low coagulation factors might be a compensatory reaction to abundant thrombin generation. It has also been reported that increased activity of thrombin activatable fibrinolysis inhibitors impairs the fibrinolytic system and that vWF is high, which could be evidenced following the Fontan procedure; pulmonary blood flow that is not a pulse wave, slow-flowing systemic veins, and hypoxia lead to endothelial dysfunction. Moreover, following the Fontan procedure in adults with a history of embolism, platelet activation has been found to increase P-selectin exposed on the membrane surface, as well as soluble CD40 ligand, and platelet activity has been found to be enhanced. This is the reason for supporting antiplatelet therapy. However, in activated endothelial cells in vascular impairment, low-dose aspirin therapy does not adequately inhibit proteins expressed by platelets, such as CD40 ligands,14) and further examination is warranted. In other words, following the Fontan procedure, it is possible that adults could have various abnormalities, such as increased platelet activation, endothelial dysfunction, increased thrombin generation, and fibrinolytic system impairment. If the bleeding as a side-effect could be overcome, then the combined administration of anticoagulants and antiplatelets might be ideal. If increased thrombin generation is a problem, then new anticoagulants, such as antithrombin agents, could be promising, and a novel platelet aggregation inhibitor that is better than aspirin also needs to be developed.
In the present study, patients who had cerebral infarction as very long-term sequelae were only those initially considered to be at a high risk, with a residual pulmonary artery stump, concurrent pulmonary arteriovenous fistula, and a history of atrioventricular valve replacement. Unfortunately, the congealing fibrinogenolysis system was not examined in detail at the time of cerebral infarction onset and the cause of thrombus formation was not examined. A residual pulmonary artery stump has been reported to be extremely dangerous,15) and the results of the present study suggested that the combined use of warfarin and aspirin could be insufficient in high-risk patients. Thus, either TEE should be performed proactively, warfarin used at a higher dose, or surgery be considered.
In the patient who died of pulmonary hemorrhage and refused to undergo contrast-enhanced angiography, back flow of the descending aorta was not confirmed on CT and echography to examine the collateral vessels. It is highly likely that the pulmonary hemorrhage was caused by abnormal collateral arteries, and we believe that cardiac catheterization should have been recommended actively. The other two patients were successfully treated by discontinuing aspirin and reducing the dose of warfarin. However, in the patient with diffuse alveolar hemorrhage, the bleeding repeated even after embolization of the abnormal vessels, and while the underlying mechanism was unclear upon initiation of low-dose macrolide therapy, a reduction in the hemoptysis was observed. In recent years, macrolides have been reported to reduce pulmonary neutrophils, reduce IL-8, and inhibit neutrophilic inflammation of the airway,16) and it is thought that they could improve pneumonopathy.
With regards to complications of gastrointestinal bleeding, in the present study, among patients administered aspirin at a low dose of 1–2 mg/kg/day combined with warfarin, some suffered ulceration that led to massive bleeding. In particular, patients with aspirin-related ulceration might not complain of abdominal pain. Among our patients, only one complained of abdominal pain. Even with mild ulceration without abdominal pain, it should be kept in mind that massive hemorrhage can result with warfarin combination therapy in particular. Enteric-coated aspirin tablets are not the ultimate treatment, and ulceration in the small intestines has been reported in recent examinations using capsule endoscopy. Among patients receiving anticoagulant and antiplatelet therapy, ulceration should be considered in those without abdominal pain, with blood in the stool, and with gastrointestinal bleeding that develops suddenly into shock. For the prevention of aspirin-related ulceration, the combined use of PPIs is a common practice, and it has been reported that PPIs with H2 blockers are effective for primary protection.17, 18) However, this issue has not been discussed in detail for pediatric cases. According to the “Clinical Practice Guidelines for Peptic Ulcers” published by the Japan Society of Gastroenterology in October 2009, PPIs are the first choice of drug, and in the treatment of stomach ulcers, it is hard initially to use H2 blockers and mucosal protective agents. While treatment should be flexible for each case, in adults considered to have no problem, there is the issue of whether gastric acid inhibition is safe over the long-term, and the examination of patients with congenital heart disease and young patients is needed.
Furthermore, it has been reported that, as an expected event, it is significantly common for adults to experience chronic venous insufficiency of the legs following the Fontan procedure.19) In the future, there is concern that in patients following the Fontan procedure, thrombotic factors will become apparent with age and increase the incidence of thrombosis. To date, physician cooperation has been needed for the above; therefore, information regarding surgical methods, hemodynamics, and expected complications should be shared.
At present, explanations are given to patients undergoing the Fontan procedure and their families indicating that TE could occur, and that in the event of the appearance of symptoms suggestive of cerebral infarction, such as paralysis, they are instructed to present to a doctor via ambulance immediately for thrombolytic therapy. They are also told that as TE preventive agents can cause hemorrhagic complications, they should check for the presence or absence of blackish feces daily. Patients receiving aspirin in combination with warfarin should proactively consider the combined use of antiulcer agents. They are also instructed as necessary that even in the absence of hemoptysis, regular cardiac catheterization and angiography are needed to examine the presence or absence of abnormal vessels. In everyday life, when diarrhea develops, they are told that because of the inhibition of vitamin K absorption, warfarin can be too effective and that antimicrobials inhibit the intestinal flora and affect metabolism, thereby increasing PT-INR. Moreover, even when PT-INR is within the therapeutic range, it is possible that small wounds may take time to stop bleeding. Therefore, it is recommended to purchase an alginate dressing that promotes hemostasis.
In the present study, gastrointestinal bleeding was common in children and youths, whereas cases at a high risk of infarction tended to be seen only in adulthood. This seems to support the discontinuation of warfarin for several years postoperatively, then recommencing the agent in adulthood. However, at present, no patients at our department have undergone follow-up observation with aspirin monotherapy. Therefore, we cannot compare the anticoagulant and antiplatelet groups. Furthermore, at our hospital, cardiac catheterization is not performed on a patient without undergoing the Fontan procedure. Therefore, pulmonary vascular resistance was not examined in detail. It does not appear to be a problem that can be solved quickly through performing further random sampling tests via an enrollment system of Fontan procedure patients and comparative studies of Fontan circulatory insufficiency, such as the detailed shift in pulmonary vascular resistance in multicenter prospective collaborative studies, and the presence or absence of thrombi by regular TEE. We hope the day will arrive when we are able to explain to patients with confidence whether warfarin should be discontinued for several years postoperatively and then recommenced in adulthood, whether aspirin and warfarin should be used for life together with PPIs and H2 blockers to prevent silent emboli and maintain good Fontan circulation, and whether a novel anticoagulant would be more effective.