The number of sudden deaths occurring under school supervision has been gradually declining from 80 to 30 per year from 1999 to 2008 in Japan. Approximately 70% of the causes of sudden death under school supervision are attributed to cardiac disease. In particular, cardiomyopathy reigns as the most common heart disease resulting in sudden cardiac death, followed by other causes such as congenital/acquired heart disease and arrhythmias. In recent years, the Japanese population has witnessed a gradual increase in the proportion of cardiomyopathy patients—with HCM representing the vast majority of the increase.1, 2) Thus, it is imperative to investigate the background of sudden death attributed to an underlying HCM and consider appropriate countermeasures to reduce the incidence of sudden cardiac death occurring under school supervision.
The installation of automated external defibrillators (AED) in public facilities including schools has been increasing since the use of AEDs by non-medical persons was approved in July 2004 in Japan. There have also been reports documenting successful interventions via the use of AED in school settings. The purpose of this study is to dissect documented cases of cardiac events attributed to HCM occurring under school supervision and examine how the interventional use of AED ultimately influenced the clinical outcome.
The subjects examined in the present study include patients who succumbed to illness or injury under school supervision/management at elementary, junior high school, high school, kindergarten and nursery school between 2004 and 2011. Approximately 97% of all school and kindergarten students in Japan are enrolled in the Mutual Aid Disaster Insurance system provided by the Japan Sports Council. The Japan Sports Council maintains a vast and highly unique database that contains virtually all cases involving injury, illness or death occurring under school supervision in Japan. The phrase “under school supervision” in this study is defined as the entire period between the moment a student walks out the front door of his/her home to go to school until the moment where he/she sets foot back inside his/her home (this includes daily school activities, school trips and extracurricular activities).2) 218 cases were classified as sudden cardiac deaths in the database and we selected specific cases in which sudden cardiac death was caused by HCM. This subset of data was designated the “non-survivor group.” Additionally, we conducted a keyword inquiry using the terms “cardiac arrest,” “AED,” “defibrillation” and “cardiomyopathy” using the same database and identified 140 cases fitting the search criteria. We subsequently analyzed these cases, selected only those in which the cardiac arrest was triggered by HCM but the individuals were successfully revived via resuscitation. We designated this subset the “survivor group.” Gender ratio, type of educational facility, time of diagnosis, availability of AED and circumstances at the time of cardiac arrest were also compared and examined to delineate any differences that exist between the survivor and non-survivor groups. For the term “sudden death” we adopted the following definition provided by the World Health Organization (WHO): “unexpected intrinsic death within 24 hours from onset.” Cases in which the victim died after a prolonged (several days to several months) state of unconsciousness or vegetation induced by the initial cardiac arrest were also included.
Baseline: Non-Survivor and Survivor Groups
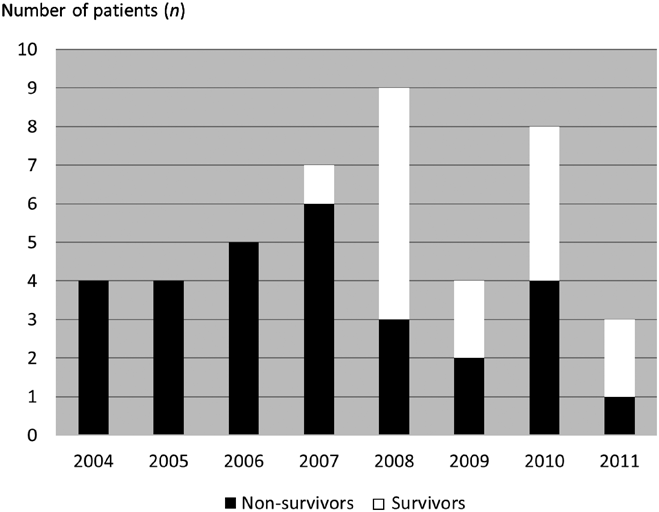
Among 218 cases of sudden cardiac death, 29 cases (13.3%) were attributed to HCM (non-survivor group). On the other end of the spectrum, among the 140 cases identified via the keyword query, 15 cases of cardiac arrest caused by an underlying HCM were successfully revived via the use of an AED or ICD (survivor group) (Table 1). For the non-survivor group, 4 cases occurred in 2004, 4 cases in 2005, 5 cases in 2006, 6 cases in 2007, 3 cases in 2008, 2 cases in 2009, 4 cases in 2010 and a single case in 2011 (Fig. 1). In the survivor group, no reports of successful resuscitation were documented prior to 2007. The annual breakdown of cases ending in successful resuscitation is as follows: 1 case in 2007, 6 cases in 2008, 2 cases in 2009, 4 cases in 2010 and 2 cases in 2011 (Fig. 1).
Table 1 Characteristics of schoolchildren with HCM | Non-survivors (n=29) | Survivors (n=15) |
|---|
| Male | 24 (83%) | 10 (67%) |
| School grade | | |
| Nursery | 1 | 0 |
| Primary school | 3 | 0 |
| Junior high school | 10 | 8 |
| High school | 15 | 7 |
Of the 29 cases resulting in death in the non-survivor group, there were no reports detailing the attempted use of an AED in 2004 or 2005. Of the 21 fatalities occurring since 2006, 14 cases (67%) were confirmed to have attempted resuscitation using an AED—the individuals operating the AED in these cases were 11 school staff members and 3 emergency medical personnel.
One case in the survivor group had been pre-diagnosed with HCM and was fitted with an ICD. The ICD operated at the onset of the cardiac event resulting in the prompt resuscitation of the individual. In the remaining 14 cases included in the survivor group, an AED was used by 12 school staff members, a guardian of another student who happened to be in the vicinity, and 1 emergency medical personnel (Table 2). We also confirmed that ICD implantation was subsequently performed after successful resuscitation and recovery in 12 cases. Within the survivor group, we confirmed that two individuals went on to continue their education without any issue and another resumed a normal course of daily activities albeit with minor limitations on physical activity. We also confirmed that another survivor was discharged from the hospital following a brief period of hospital admission; however, what followed after the initial successful resuscitation in the remaining 12 cases is unknown as follow-up information was not available.
Table 2 Circumstances during cardiac events | Non-survivors (n=29) | Survivors (n=15) |
|---|
| Pre-diagnosed HCM | 14 (48%) | 3 (20%) |
| Situation | | |
| Exercise | 16 | 14 |
| Moving, free time | 6 | 1 |
| Going to school/home | 5 | 0 |
| Classroom, lecture | 1 | 0 |
| Sleep/nap time | 1 | 0 |
| AED operation | | |
| 2004–2005 | 0/8 | 0 |
| 2006–2011 | 14/21 (67%) | 14/15* |
| *One student had a previous incident in which the ICD was activated. |
Comparison between Non-Survivor vs Survivor Cases
The ratio between males and females was 24 : 5, 10 : 5 for the non-survivor and survivor groups, respectively, with a significantly higher number of boys in comparison to girls in either group (Table 1). With regard to the type of educational facility in which cardiac fatalities took place, 1 case occurred in a nursery school, 3 in elementary school, 10 in junior high school and 15 in high school (Table 1). Specifically, the deaths occurred in 1 nursery school student, 1 first-grader in elementary school, 2 sixth-graders in elementary school, 4 first-year junior high school students, 3 second-year junior high school students, 3 third-year junior high school students, 3 first-year high school students, 5 second-year high school students and 7 third-year high school students. In the survivor group, 8 cases occurred at junior high school, 7 in high school, and no cases were documented in nursery or elementary schools (Table 1). Specifically, cardiac events not resulting in fatalities occurred in 1 first-year junior high school student, 5 second-year junior high school students, 2 third-year junior high school students, 2 first-year high school students, 2 second-year high school students and 3 third-year high school students. In order to preserve the privacy of these minors, the actual age of the children is withheld when data is released—age is recorded at the time of registry but is known only to the Japan Sports Council.
Fourteen cases (48%) in the non-survivor group and 3 cases (20%) in the survivor group were diagnosed with HCM prior to the onset of cardiac events (Table 2). With regard to the remaining cases that were not pre-diagnosed with HCM, 3 of the 15 cases in the non-survivor group showed no abnormalities on ECG during a standard cardiac check-up, while another individual showed an incomplete right bundle branch block (IRBBB) and premature ventricular contractions (PVC). For the remaining 11 cases, the status of standardized cardiac check-ups was unknown. Of the 12 cases in the survivor group that were not diagnosed with HCM, 2 individuals showed no abnormalities on ECG during a standard cardiac check-up and the remaining 10 individuals had unknown status with regard to the results of their standard cardiac check-up. It should be noted that the records of the standard cardiac check-ups conducted in school children only retain the final diagnosis and or findings identified by the examining physician and therefore no copies of the ECGs were available for review by the authors.
With exception to one individual in the non-survivor group, the School Life Guidance and Management Form was reviewed for every individual who received a diagnosis for HCM and it was confirmed that each individual had been placed on restrictions for physical activity. Instruction category (i.e., the amount of physical exertion deemed appropriate for each child stratified into six categories, A through E+), along with the type of physical activity each child was engaged in at the time of the cardiac event has been summarized in Table 3. For the 14 individuals with HCM diagnosis the number of individuals per “instruction category” are as follows: Category B, 5 individuals; Category C, 3 individuals, Category D, 3 individuals; Category E−[sports club activity not allowed], 1 individual; Category E+[sports club activity allowed], 1 individual; unknown, 1 individual. 11 cases (78.6%) fall under Categories B–D (i.e., restricted physical activity) but only one individual suffered a cardiac event during exercise. Within the survivor group one individual was assigned a Category C and 2 individuals a Category D—cardiac events transpired during exercise in these 3 individuals.
Table 3 Level of exercise restriction and activity engaged in at the time of the cardiac event| Restriction level (Non-survivor/Survivor) | Exercise (n=7) | Moving, free time (n=5) | Going to school/home (n=5) | Total (n=17) |
|---|
| B (5/0) | 0/0 | 2/0 | 3/0 | 5 |
| C (3/1) | 0/1 | 2/0 | 1/0 | 4 |
| D (3/2) | 1/2 | 1/0 | 1/0 | 5 |
| E (2/0) | 2/0 | 0/0 | 0/0 | 2 |
| Unknown (1/0) | 1/0 | 0/0 | 0/0 | 1 |
B: Restriction of mild or stronger exercise
C: Restriction of moderate or stronger exercise
D: Restriction of strenuous or competitive exercise
E: No exercise restriction |
In the non-survivor group, 16 individuals experienced cardiac events during exercise, 6 during recess/passing period, 5 during going to school, 1 during classroom instruction and 1 during nap time. In the survivor group, 14 individuals experienced cardiac events during exercise and 1 during recess/passing period. In both groups, the majority of cardiac events occurred during exercise (Table 2). Upon closer examination of the type of exercise the individuals were engaged in at the time of the cardiac event in the non-survivor group, 8 individuals were running (including warm-ups, light jogging, long-distance running, etc.) and 8 were playing ball games (soccer, 4 individuals; basketball, 2 individuals, volleyball; table tennis, 1 individual). In the survivor group, 13 individuals experienced cardiac events during runs and 1 during a game of tennis.
HCM is not an uncommon disease with a reported prevalence in Japan and the US of 374/100,000 and 170/100,000 population, respectively.3–5) It is also the leading cause of sudden cardiac death in young adults and therefore is a capital issue to address in any sudden death prevention strategies in this particular demographic.6–8) A major epidemiological study conducted in Japan in 2002 reported the annual mortality rate for HCM at 2.8%—the cause of death was an arrhythmia in 31.9% and heart failure in 21.3% of cases.3, 9) A study conducted by Maron et al on sports-related sudden death in young adults/children identified the most common cause as HCM which accounted for 26.4% of cases.10) Another recent study conducted in Japan examined 58 cases of cardiac arrest occurring in young adults outside of the hospital setting and identified 8 cases in which HCM was the primary cause, of which cardiac arrest occurred at school in 6 cases and in 4 cases during or after exercise.11) Pilmer et al histologically examined cases of sudden cardiac death occurring in ages 1 through 19 in Canada between 2005 and 2009 and diagnosed HCM in 8 out of 56 cases (14%).12) In the present study, we identified a total of 218 cases of sudden cardiac death that occurred under school supervision, of which HCM fatalities accounted for 29 cases (13.3%). In comparison to earlier years, the present data suggests a slight reduction in the proportion of sudden cardiac deaths caused by HCM. A clear gender predisposition was also revealed in cases where cardiac events were induced by HCM, whereby the ratio of boys was significantly higher than girls in both the survivor and non-survivor groups. In both groups, the highest incidence of cardiac events occurred in high school students.
The present study examined cases enrolled in the Mutual Aid Disaster Insurance database maintained by the Japan Sports Council. Virtually all school students (approximately 97%) in Japan are enrolled in this database which allows us unique insight into trends occurring at the national level. Prior to July 2004, only medical personnel were allowed to operate an AED in Japan, but since then non-medical staff including school staff members have been permitted to use AEDs and with that the proliferation of AED usage and availability has expanded nationally. While the use of AEDs during cardiac events occurring under school supervision in students diagnosed with HCM prior to and including 2006 has been documented, none of these cases ended in successful resuscitation of the patient. Successful resuscitation using AEDs was only reported from and after 2007. With exception to one case in which the student had an ICD, all students who were diagnosed with HCM in the survivor group were applied AEDs following the onset of cardiac events. While there were a number of cases ending in fatalities regardless of the use of an AED, it should be noted that all cases without AED or ICD intervention ended in fatalities. Although the timing in which AED intervention was attempted and time required to transport the victim to a healthcare facility are important factors to consider as they directly influence the outcome in each case, no such data was available for review and analysis. Moving forward, the contents of the Japan Sports Council’s database should be amended to include such information so that these parameters may be evaluated in order to identify new measures to improve the existing framework on the usage of AED.
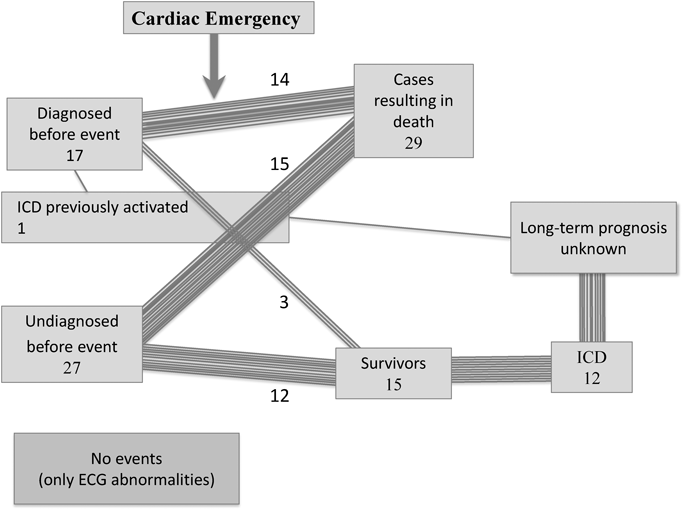
Upon closer examination of cardiac events occurring in children, 14 (48%) and 3 (20%) cases were diagnosed with HCM in the non-survivor and survivor groups, respectively (Fig. 2). The proportion of confirmed HCM patients was significantly higher in the non-survivor group and thus urges the need for enhanced monitoring on clinical progression and aggressive prevention strategies in patients who have been diagnosed earlier on in life. Additionally, a thorough review of the School Life Guidance and Management Form for each individual diagnosed with HCM in the non-survivor group showed 11 individuals were assigned a “B”, “C”, or “D” instruction category (i.e., limited physical activity). Within this subset of 11 individuals, cardiac events occurred during exercise in only a single individual while the remaining individuals experienced cardiac events during passing period, classroom instruction or on their ways to school. Thus, despite the virtually flawless adherence to restrictions on physical activity, cardiac events still occurred, which collectively suggests the severity of the underlying condition and the inevitability of onset regardless of any restrictions in place. While there is no direct evidence to support this theory, it is imperative that adults tasked with the supervision of children with severe cases of HCM understand that cardiac events can occur at any time regardless of the presence or absence of appreciable triggers. Two individuals in the non-survivor group were assigned an instruction category of “E”, and two in the survivor group were assigned “C” and “D”, respectively. All of these individuals experienced cardiac events during exercise and by verifying the specific conditions in which these events took place with witnesses and school staff it could culminate in the prevention of future events. We were able to confirm that in one individual (no irregularities documented during cardiac check-up) the instruction category was escalated to an “observe only” status after recovery from the initial cardiac event. This individual was only allowed to observe and not participate in physical education after suffering the initial cardiac event. In the remaining cases, it is unknown if such escalation took place, however, it is important for school staff, parents and guardians and primary care physicians to discuss strategies to minimize the risk of such occurrences.
The type of physical exertion the individuals were engaged in at the time of exercise varies considerably; however, the most common form of exertion during which cardiac events occurred was running. In any sports, running is the top contender for the longest continuous activity occurring over extended durations. Meanwhile, 50% of cases in the non-survivor group were engaged in ball games at the time of onset while only 7.1% of cases were engaged in the same activity. The reason for this remains unknown although the argument can be made that ball games could simply entice a participant to continue physical exertion over longer periods of time than simply running because of the enjoyment factor.
A combined total of 27 cases from both groups were only diagnosed with HCM after a cardiac event suggesting that the manifestation of symptoms can be abrupt rather than gradually progressive. The data observed in this study indicates the rapid and immediate intervention of a cardiac event using an AED is of critical importance to the prognosis. According to the “Current status of AED deployment in school” published by the Ministry of Education, the percentage of elementary, junior high and high schools with active or proposed implementation in 2010 was 96.4%, 99.8% and 99.2%, respectively. Including kindergartens, this translates into 85.4% of all schools in Japan13) that currently have or will have AEDs available on-site. There has, however, been criticism regarding the lack of the number of units deployed and their specific locations at each site.14)
In one case included in the survivor group it was confirmed that an ICD had been implanted prior to the cardiac event. In the remaining 12 out of 14 cases we confirmed that an ICD was implanted following the cardiac event (Fig. 2). Although the Guidelines for Diagnosis and Treatment of Patients with Hypertrophic Cardiomyopathy (JCS 2012)3) published by the Japan Circulation Society (JCS) addresses the indications for ICD implants that can be applied to pediatric cases, no specific indications exist for children in the current guidelines. A recent study including 224 pediatric HCM cases who had undergone ICD implantation showed that over an average period of 4.3 years, the ICD delivered a shock in 43 (19%) individuals suffering from ventricular tachycardia or ventricular fibrillation. However, on the opposite end of the spectrum, the same study reported inappropriate shocks, lead failures and other complications in 91 (41%) patients.15) Another study included 73 HCM patients who underwent ICD implantation for prevention of SCD before the age of 30 at five institutions across the United States between 1995 and 2009. The investigation concluded that appropriate shocks occurred in 11 cases (shock delivered in 8 (11%) cases, anti-tachycardia pacing in 3 (4%) cases) patients. Inappropriate shocks, however, occurred in 16 (22%) cases.16) This is not an isolated report as others have clearly documented the role of ICDs significantly reducing the risk of sudden death in young HCM patients, but at the concomitant risk of offering lead failures and other disadvantages to patients.17, 18) Only a limited number of investigations on the subject of ICD implantation in young HCM patients exist in Japan,19) but further investigations are required to overcome the current notion that ICDs serve exclusively as a means to prevent sudden cardiac death, broaden the indications for ICDs in young HCM patients and expand on safeguards to preserve the best interest of patients.
There are a number of limitations associated with the present study that should be addressed. First, the study is retrospective in nature and therefore has an inherent limitation owing to the study type. Secondly, the initial search was conducted based on a keyword query and thus this carries the possibility of cases being inadvertently passed over due to a lack of “hits” using the defined search criteria. Third, non-medical staff (in most cases the teacher) are also allowed to record the events and circumstances under which an incident occurred and therefore the remarks are at times incomplete. Additionally, while the diagnosis for each child is conducted by a physician, the detailed reports leading up to the diagnosis along with relevant data (e.g., ECG, lab data, etc.) is rarely provided to the Japan Sports Council and therefore we were unable to review ECG and other medical records in detail. Therefore, the cases we accumulated are based solely on the diagnosis provided by the initial diagnosing physician. In many cases we were able to identify and confirm records of individuals having an ICD implanted following the cardiac event. Unfortunately, we were unable to conduct further follow-ups on the presence of any neurological impairment nor confirm whether or not the ICDs intervened in later months/years in these individuals. The strength and novelty of the present study lies in the rarity of reports specifically addressing the issue of cardiac events occurring in schoolchildren under school supervision. The present study further elucidates the reality and importance of AEDs in preventing sudden cardiac death and paves the path for future investigations into the subjects of strategic AED deployment, cardiopulmonary resuscitation (CPR) training and prognosis for ICD-implanted patients.
HCM is a life-threatening condition and is one of the leading causes of sudden cardiac death in children and young adults. Since the use of AEDs by non-medical persons became commonplace, the number of victims who have been successfully revived after suffering from cardiac arrests under school supervision has increased. The present study demonstrates the effectivity of AEDs and ICDs in the prevention of sudden cardiac death in the public domain and echoes the plea for enhanced deployment strategies, widespread recognition and expanded applications.
Note
The abstract was presented at the 50th Annual Meeting of the Japanese Society of Pediatric Cardiology and Cardiac Surgery.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Originally published in Pediatric Cardiology and Cardiac Surgery, Vol.31 (2015)No. 5, pp. 240–245.
引用文献References
1) Ayusawa M: Current events of interest in school insurance: Exploring the reality of sudden death under school supervision. J Child Health 2014; 73: 272–276 (in Japanese)
2) Ayusawa M, Ito S, Okada K, et al: Imperatives in preventing sudden death under school supervision, Dai 2-han, 1 satsu, Tokyo, 2011, National Agency for the Advancement of Sports and Health (in Japanese)
3) Doi Y, Ichida F, Kawai H, et al: Guidelines for the diagnosis and treatment of cardiovascular disease (Joint Working Group Report 2011), Guidelines for Diagnosis and Treatment of Patients with Hypertrophic Cardiomyopathy (JCS 2012). http://www.j-circ.or.jp/guideline/pdf/JCS2012_doi_h.pdf
4) Kuroda T, Shina A, Tsuruta K, et al: Mass screening of cardiovascular disorders by two-dimensional echocardiography. J Cardiol 1989; 19: 933–943
5) Maron BJ, Gardin JM, Flack JM, et al: Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA study. Coronary Artery Risk Development in (Young) Adults. Circulation 1995; 92: 785–789
6) Maron BJ, Epstein SE, Roberts WC: Hypertrophic cardiomyopathy: A common cause of sudden death in the young competitive athlete. Eur Heart J 1983; 4 Suppl F: 135–144
7) Maron BJ, Haas TS, Murphy CJ, et al: Incidence and causes of sudden death in U.S. college athletes. J Am Coll Cardiol 2014; 29: 1636–1643
8) Maron BJ, Haas TS, Ahluwalia A, et al: Incidence of cardiovascular sudden death in Minnesota high school athletes. Heart Rhythm 2013; 10: 374–377
9) Matsumori A, Furukawa Y, Hasegawa K, et al:Co-research workers: Epidemiology and clinical characteristics of cardiomyopathies in Japan: Results from nationwide surveys. Circ J 2002; 66: 323–336
10) Maron BJ: Sudden death in young athletes. N Engl J Med 2003; 349: 1064–1075
11) Mitani Y, Ohta K, Ichida F, et al: Circumstances and outcomes of out-of-hospital cardiac arrest in elementary and middle school students in the era of public-access defibrillation. Circ J 2014; 78: 701–707
12) Pilmer CM, Kirsh JA, Hildebrandt D, et al: Sudden cardiac death in children and adolescents between 1 and 19 years of age. Heart Rhythm 2014; 11: 239–245
13) Ministry of Education: A survey on the status of current deployment of AEDs in schools (Current deployment as of end of March 2010 and current plans for the deployment of AEDs throughout 2010). http://www.mext.go.jp/a_menu/kenko/anzen/1339095.htm
14) Mitamura H, Takayama M, Iwami T, et al: Specific recommendations for the setting and deployment of ARDs. Shinzo 2012; 44: 392–402 (in Japanese)
15) Maron BJ, Spirito P, Ackerman MJ, et al: Prevention of sudden cardiac death with implantable cardioverter-defibrillators in children and adolescents with hypertrophic cardiomyopathy. J Am Coll Cardiol 2013; 61: 1527–1535
16) Kamp AN, Von Bergen NH, Henrikson CA, et al: Implanted defibrillators in young hypertrophic cardiomyopathy patients: A multicenter study. Pediatr Cardiol 2013; 34: 1620–1627
17) Kaski JP, Tomé Esteban MT, Lowe M, et al: Outcomes after implantable cardioverter-defibrillator treatment in children with hypertrophic cardiomyopathy. Heart 2007; 93: 372–374
18) Schinkel AF, Vriesendorp PA, Sijbrands EJ, et al: Outcome and complications after implantable cardioverter defibrillator therapy in hypertrophic cardiomyopathy: Systematic review and meta-analysis. Circ Heart Fail 2012; 5: 552–559
19) Suzuki T, Sumitomo N, Yoshimoto J, et al: Current trends in use of implantable cardioverter defibrillators and cardiac resynchronization therapy with a pacemaker or defibrillator in Japanese pediatric patients: Results from a nationwide questionnaire survey. Circ J 2014; 78: 1710–1716