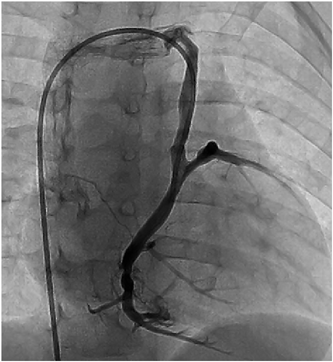
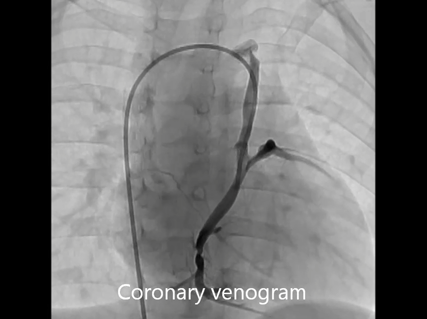
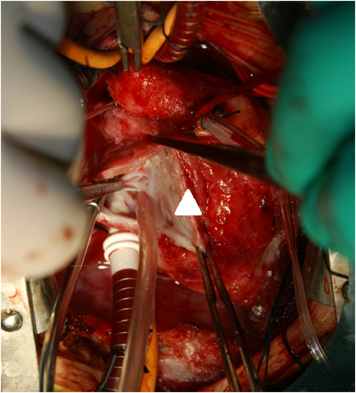
Coronary Sinus Orifice Atresia in Tricuspid Atresia
Hiromitsu Shirozu1,Jun Muneuchi1,Yusaku Nagatomo1,Mamie Watanabe1,Seigo Okada1,Chiaki Iida1,Yoshie Ochiai2Hiromitsu Shirozu1, Jun Muneuchi1, Yusaku Nagatomo1, Mamie Watanabe1, Seigo Okada1, Chiaki Iida1, Yoshie Ochiai2
1 Department of Pediatrics, Japan Community Healthcare Organization Kyushu Hospital ◇ Fukuoka, Japan
2 Department of Cardiovascular Surgery, Japan Community Healthcare Organization Kyushu Hospital ◇ Fukuoka, Japan
受付日:2017年8月14日Received: August 14, 2017
受理日:2018年2月23日Accepted: February 23, 2018
発行日:2018年7月1日Published: July 1, 2018