Few studies have examined the coronary arterial calcification (CAC) which develops after the acute phase of Kawasaki disease (KD) and narrows the coronary arterial lumen, increasing the risk of acute coronary syndrome.1) Pathological examination of KD-induced coronary arterial lesions thus far has been limited to autopsy cases, and no studies have reported on the composition analysis of CAC.
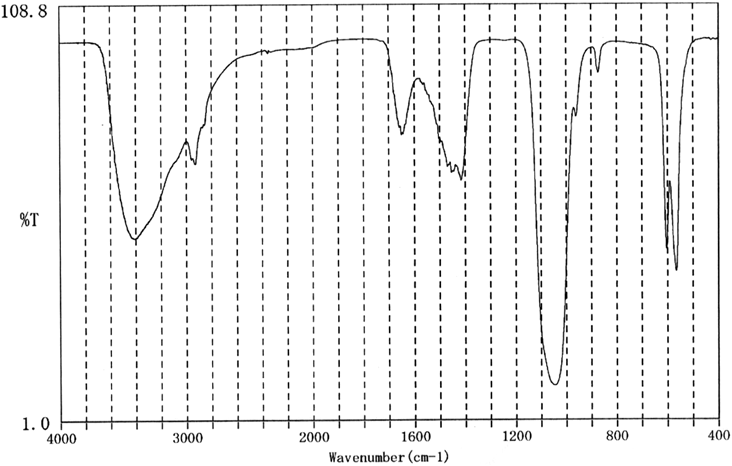
We can use various methods to analyze compositions of materials. Infrared absorption spectrometry is an analysis technique for analyzing compositions of materials such as urinary stones using infrared radiation.2) When infrared radiation is applied to materials, it is reflected or is transmitted. Measuring quantities of these infrared radiation allows us to conduct the compositions of materials, because quantities of reflected/transmitted infrared radiation are specific to each chemical structure of materials. Dual-energy CT is an imaging device which uses two different energy level X-rays to evaluate the grafts. This type of CT allows us to obtain the effective atomic numbers (EANs) of materials, which are particular atomic numbers calculated from the ratio of amplitude and frequency of X-rays penetrating materials. EANs allow us to obtain the compositions of materials.3)
We herein present the case of a patient with KD-induced CAC, in whom we conducted a composition analysis of CAC with infrared absorption spectrometry and dual-energy CT.
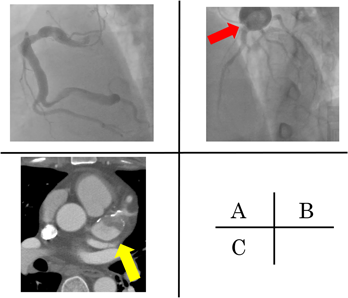
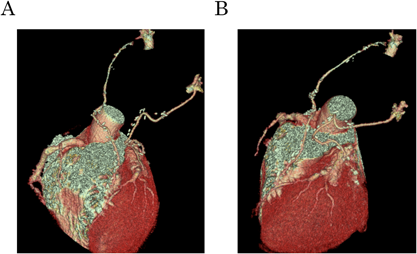
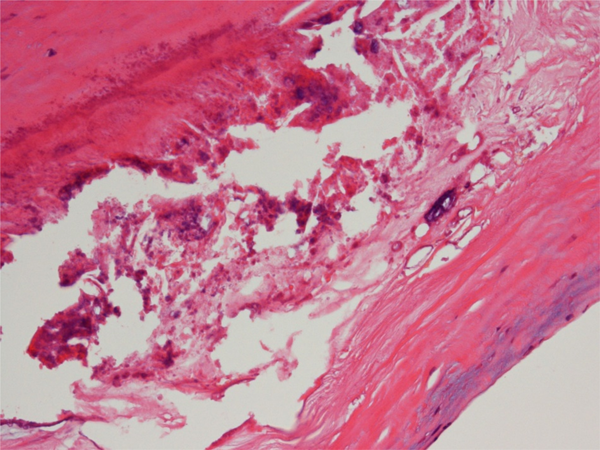
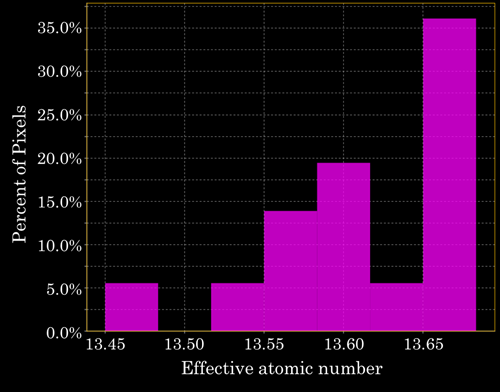
A 38-year-old man, diagnosed with KD at age 7, was admitted to our hospital with a giant coronary aneurysm. Medical data on the initial KD diagnosis were not available. However, the coronary angiography at 2 years old showed that coronary aneurysms were observed at segment 1, 2 and 5. He was treated at our hospital until the age of 13, but there were no hospital visits since then. At his current admission, he was transported to previous hospital because of sudden chest pain. The blood test showed that creatine phosphokinase was 638 IU/L and an asynergy at inferior wall was observed with echocardiography while the cardiac function was normal. T-wave abnormality or the other specific findings of acute coronary syndrome were not seen with electrocardiogram. He was suspected with myocardial infarction. With the coronary angiography, the right coronary artery was dilated on the whole and a giant coronary aneurysm was observed at the left coronary artery while there were no stenoses (Fig. 1A, B). His condition improved with heparin and nicorandil and he was discharged under the treatment with oral clopidigrel and warfarin. Two weeks later, he complained of chest pain again, and was transported to the hospital. The blood test showed not elevated creatine phosphokinase but slightly elevated troponin T. The cardiac CT had located a giant coronary aneurysm, three calcified lesions, and the obstruction of a coronary artery by a thrombus. His Agatston score, which assesses the severity of CAC using the cardiac CT calculated with the CT levels more than 130 HU and their areas, and which is strongly associated with the cardiovascular event onset, was 1622.5 (left main trunk, 1579.4; left circumflex coronary artery, 0; left anterior descending artery, 0; right coronary artery, 43.1) (Fig. 1C).4, 5) He was diagnosed with myocardial infarction again. After his symptom rapidly improved with heparin and nicorandil, he was transferred to our institution for the operation. At the time of admission, his body weight was 113 kg, with a body mass index of 36.9 kg/m2. His morbid obesity was complicated with hypertension (systolic/diastolic blood pressure, 146/45 mmHg at admission), which we treated with 20 mg/day of azilsartan medoxomil; and hyperlipidemia (total serum cholesterol, 155 mg/dL; total serum triglycerides, 349 mg/dL) which we treated with 5 mg/day of rosuvastatin. The patient underwent a thrombectomy and coronary artery bypass grafting (left internal thoracic artery to obtuse marginal coronary artery and right internal thoracic artery to left anterior descending artery, segment 8) (Fig. 2). The giant aneurysm was removed because it triggered blood clots and they flowed into the periphery of the coronary artery, which caused myocardial infarction during surgery. Pathological examination revealed atherosclerosis-like lesions, including the accumulation of foam cells, hyalinization, cholesterol clefts, and granular calcification (Fig. 3). After surgery, carotid ultrasonography and pulse wave velocity results were normal, which indicated that the patient did not have atherosclerotic lesions or calcifications in the other arteries. Composition analysis with infrared absorption spectrometry revealed that the CAC was composed of >98% calcium phosphate with carbonate, similar to carbonate apatite (Fig. 4). The dual-energy CT showed that the median EANs of the calcifications was 13.41 (11.14–16.38), which resembled the EAN of CAC caused by atherosclerosis, 13.8 (Fig. 5).6) These results indicated that the composition of KD-induced CAC was similar to that of atherosclerosis. The patient has not exhibited any complications after the surgery, as confirmed by a post-operative follow-up of 6 months.
We reported that the composition of KD-induced CAC resembled that of atherosclerosis, based on EANs obtained from the dual-energy CT. This result indicates that the composition and the underlying mechanism of disease progression are similar between KD and atherosclerosis.7) The EAN of CAC in the present case was similar to that in our previous study.7) Furthermore, atherosclerosis-like lesions were observed during the pathological examination, and the calcification composition resembled that of atherosclerotic lesions. These results support the possibility that the composition of KD-induced CAC resembles that of atherosclerosis, and that the mechanisms of progression are similar, with calcification developing in smooth muscle cells that differentiate into osteoblasts, like in bone metabolism.7, 8)
However, in this case, the carotid artery analysis with ultrasonography and pulse wave velocity was normal. This suggests that the arterial calcification caused by KD was formed on parts already damaged in the past, prior to arteriosclerosis. The inflammation in the acute phase of KD had significantly destroyed the structure of the coronary arteries, where atherosclerosis might subsequently occur early, and CACs were formed in the late period.9) These findings suggest that patients with the past of KD, especially with KD-induced CAC, are easy to develop atherosclerosis and they should take care of the risk factors of atherosclerosis, such as hypertension, hyperlipidemia, smoking, obesity, and diabetes.
Although, these changes of arteries can be the final results of inflammation, histological features between KD and atherosclerosis cannot be difference finally. However, our case indicates that patients with a history of KD, especially those with KD-induced CAC, are more likely to develop atherosclerosis earlier, and suggests that attention should be paid to risk factors for hardening.
引用文献References
1) Nakamura Y, Aso E, Yashiro M, et al: Mortality among persons with a history of Kawasaki disease in Japan: Mortality among males with cardiac sequelae is significantly higher than that of the general population. Circ J 2008; 72: 134–138
2) Yuzawa M, Nakano K, Kumamaru T, et al: Is the crystal component of the human urinary calculus including carbonate calcium carbonate? Int J Urol 2008; 99: 681–687 (in Japanese)
3) Matsumoto M, Takayama N: Material identification from X-ray images made with energy-differentiation type radiation line sensor. Bull Soc Photogr Imag Japan 2009; 72: 399–405 (in Japanese)
4) Agatston AS, Janowitz WR, Hildner FJ, et al: Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827–832
5) Valenti V, Ó Hartaigh B, Heo R, et al: A 15-Year warranty period for asymptomatic individuals without coronary artery calcium: A prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 2015; 8: 900–909
6) Matsui K, Machida H, Mitsuhashi T, et al: Analysis of coronary arterial calcification components with coronary CT angiography using single-source dual-energy CT with fast tube voltage switching. Int J Cardiovasc Imaging 2015; 31: 639–647
7) Kusano N, Inamura N, Marutani S, et al: Composition of coronary arterial calcifications following Kawasaki disease as determined by single-source dual-energy computed tomography. J Pediatr Cardiol Card Surg 2018; 2: 37–42
8) Demer LL, Tintut Y: Mineral exploration: Search for the mechanism of vascular calcification and beyond: The 2003 Jeffrey M. Hoeg Award lecture. Arterioscler Thromb Vasc Biol 2003; 23: 1739–1743
9) Takahashi K, Oharaseki T, Naoe S, et al: Neutrophilic involvement in the damage to coronary arteries in acute stage of Kawasaki disease. Pediatr Int 2005; 47: 305–310