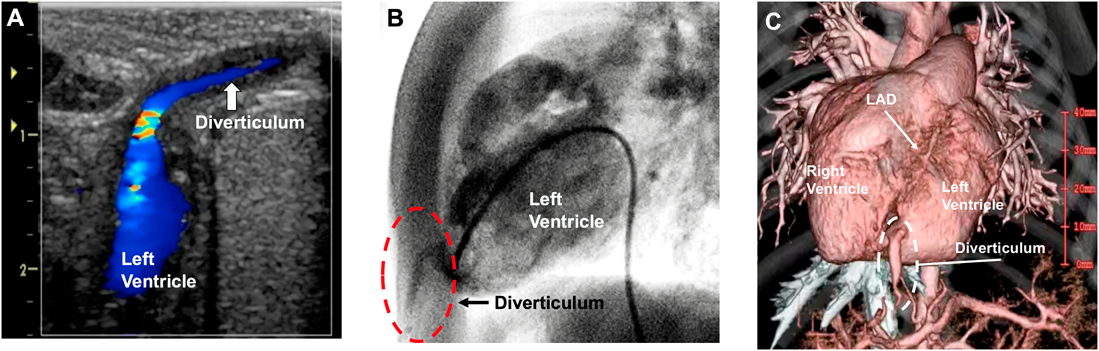
Surgical Repair of Congenital Left Ventricular Diverticulum
1 Departments of Cardiovascular Surgery, Japan Community Health Care Organization (JCHO), Kyushu Hospital ◇ Fukuoka, Japan
2 Pediatric Cardiology, Japan Community Health Care Organization (JCHO), Kyushu Hospital ◇ Fukuoka, Japan