A 30-year-old Japanese woman was referred to our obstetric department for the management of labor at 30 weeks of gestation. She was in her first pregnancy and she had been infertile for 7 years for uncertain reasons before the last surgical treatment which took place 1 year before the pregnancy.
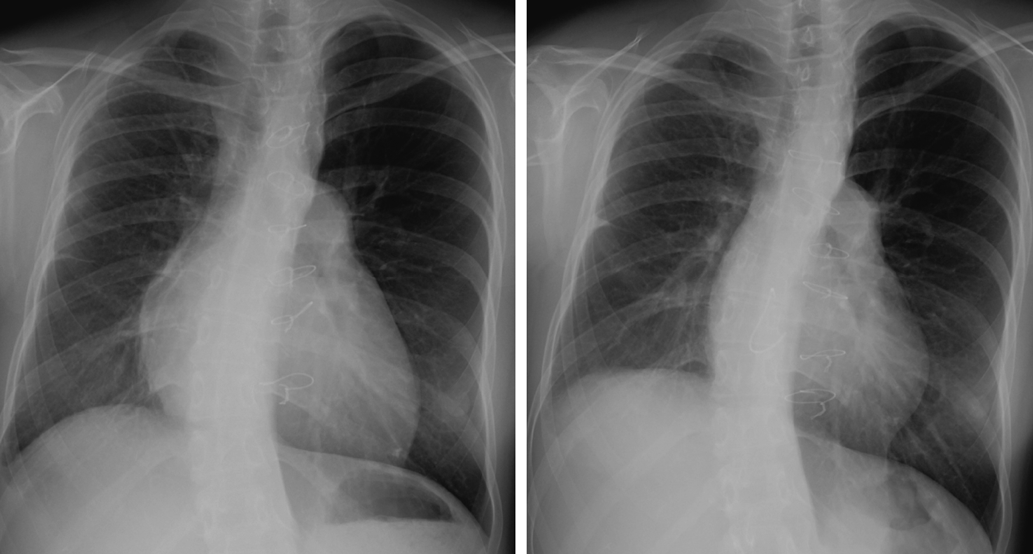
Her clinical record presented the first surgical treatment of ALCAPA using Takeuchi repair when she was one-month-old. She then underwent the following reoperations at the previous hospital: (1) residual coronary shunt closure in the reconstructed root with mitral repair when she was 1 year old; (2) the right pulmonary arterial plasty when she was 2; and (3) residual coronary shunt closure with the right ventricular outflow tract (RVOT) reconstruction using a tissue engineering patch when she was 14. However, a large patch without a leaflet caused severe pulmonary regurgitation (PR) with enlarged RV, resulting in severe tricuspid regurgitation (TR) caused by tricuspid annular dilatation. Six months before the pregnancy, she took another operation in our hospital when she was 29 year old. An expanded polytetrafluoroethylene (ePTFE) valved conduit, 22 mm of internal dimension, was used for PR repair and the Contuor 3D annuloplasty ring (Medtronic, Minneapolis, MN, USA) was applied for TR repair. The overall outcome of the RVOT reconstruction and the tricuspid valve plasty was excellent. The cardiothoracic ratio on chest X-ray was 59% and 50% before and 3 months after the operation, respectively (Fig. 1). Analogously, RV end-diastolic volume index by cardiac magnetic resonance (CMR) imaging improved from 189 mL/m2 to 64.2 mL/m2, and RV end-systolic volume index from 78.3 mL/m2 to 24.6 mL/m2. PR fraction improved from 43.4% to 4.5% (movie 1, 2). Cardiac output index increased from 1.7 L/min/m2 to 3.51 L/min/m2 calculated in CMR through the operation.
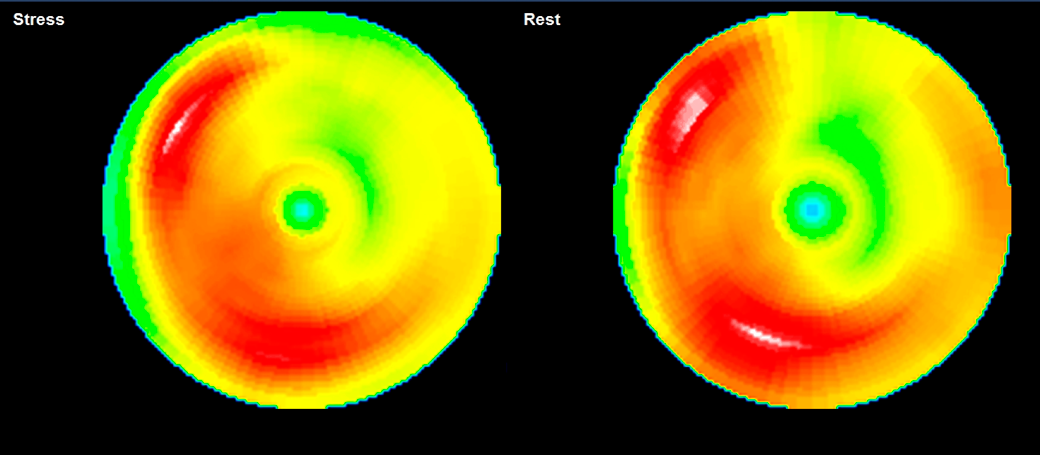
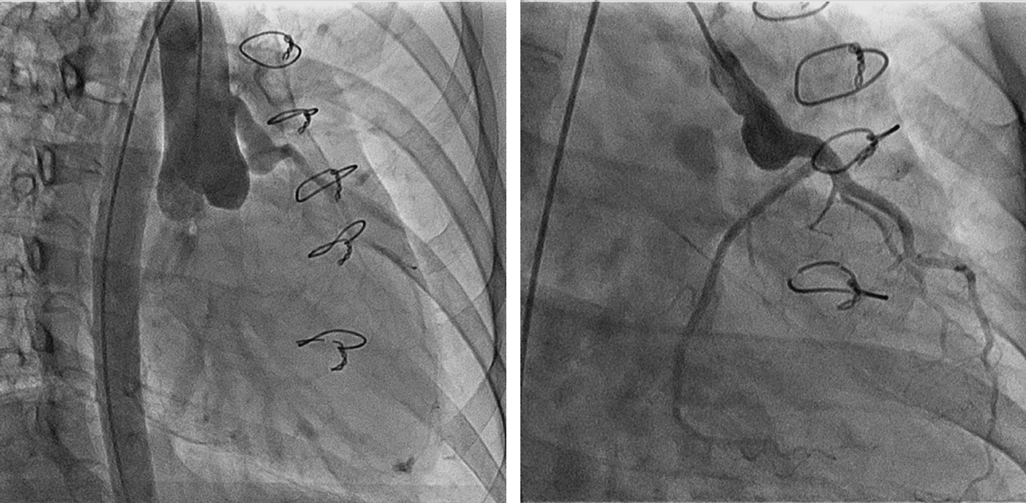
The postoperative medications including warfarin for 3 months and aspirin for 6 months as anticoagulant and antiplatelet therapies after the valve replacement were completed when she got pregnant. While, the preoperative examinations indicated good LV performance and sufficient myocardial blood supply to the coronary arteries. A myocardial perfusion scintigraphy using Technetium-99 m-labeled tetrofosmin did not indicate any significant ischemic changes both at rest and under stress (Fig. 2) with a good LV ejection fraction (LVEF) of 64%. A coronary angiography revealed a smooth blood flow through the Takeuchi route (Fig. 3).
The fetal growth was in line with the gestational age and the pregnant course was good. Her first visit to our obstetric department reported vital signs within normal ranges.
The medical team reached the consensus of aiming at painless vaginal delivery based on the patient’s request and with a view to the relief of cardiac stress during the labor.
The patient was presented for induction of labor at 39 weeks with pain control using remifentanil as planned. The vaginal delivery was successful and a healthy male baby weighed 3,062 g was born. The patient did not present any heart attack symptoms during the labor and delivery. The careful monitoring revealed a transient sinus tachycardia up to 140 bpm and systemic hypertension up to 180 mmHg followed by a smooth recovery after the delivery. The patient and the newborn were discharged on the 6th post-delivery day after normal peripartum care in our hospital.
Sequential cardiac assessments including blood examinations, echocardiography using the ACUSON SC2000™ (Siemens, Munich, Germany) ultrasound system and electrocardiography were executed during the pregnancy and for 7 months after the delivery (Table 1). The electrocardiography did not show any significant ischemic changes or arrhythmias in this period. The serum value of brain natriuretic peptide (BNP) was 21.8 pg/mL before the pregnancy and slightly elevated during the pregnancy to 49.6 pg/mL at the 37 weeks of gestational age, followed by an improvement to 25.0 pg/mL 3 days after the delivery. During the observation, The LVEF also kept adequate values around 65% and the left ventricular end-diastolic internal diameter (LVIDd) remained in the normal range, around 45 mm. E-wave velocity, A-wave velocity and E/e’ lateral ratio did not show remarkable changes. No significant insufficiencies or stenoses of atrioventricular valves and arterial valves were detected. The global longitudinal strain of LV (GLS-LV) did not deteriorate during the delivery, staying around −23% and in the normal range till 7 months after the delivery.
Table 1 Parameters of echocardiography and B-type natriuretic peptide | Before the pregnancy | 1 month before the delivery | 2 days after the delivery | 1 month after the delivery | 3 months after the delivery | 7 months after the delivery |
|---|
| LVEF (%) | 53 | 65 | 65 | 68 | 79 | 58 |
| LVIDd (mm) | 37 | 43 | 47.7 | 41.3 | 49.9 | 44.2 |
| E wave (m/s) | 1.26 | 1.6 | 1.44 | 1.2 | 1.6 | 1.2 |
| A wave (m/s) | 0.59 | 0.8 | 0.6 | 0.5 | 0.4 | 0.7 |
| E/e’ lateral ratio | | 10.1 | 10.2 | 11.5 | 11 | 8 |
| GLS-LV (%) | | −19.8 | −25 | | −25.9 | −27.4 |
| FAC-RV (%) | 30 | 58.3 | 25.4 | 57.1 | 60.4 | 40.6 |
| TAPSE (mm) | | 17.3 | 20 | 23.4 | 22.7 | 10.7 |
| TDI-S’ wave velocity (mm/s) | 4.6 | 9.8 | 7.9 | 5 | 8 | 6.8 |
| LS-fwRV (%) | | −19.7 | −10.7 | −23.8 | −30.6 | −14.8 |
| BNP (pg/mL) | 21.8 | 49.6 | 25 | | 25.5 | 40.9 |
| A wave, mitral inflow A wave; BNP, B-type natriuretic peptide; E wave, mitral inflow E wave; FAC-RV, ractional area change of right ventricle; GLS-LV, global longitudinal strain of left ventricle; LS-fwRV, right ventricular longitudinal strain only from the free wall; LVEF, left ventricular ejection fraction; LVIDd, left ventricular end-diastolic internal diameter; TAPSE, tricuspid annular plane systolic excursion; TDI-S’ wave velocity, tissue doppler imaging-derived tricuspid lateral annular systolic wave velocity. |
Fractional area change of RV (FAC-RV), tricuspid annular plane systolic excursion (TAPSE), tissue doppler imaging derived tricuspid lateral annular systolic wave velocity (TDI-S’ wave velocity) and the RV longitudinal strain only from the free wall (LS-fwRV) were used for the estimation of RV function. Monitoring results indicated that FAC-RV (LS-fwRV) deteriorated from 58.3% to 25.4% (−19.7% to −10.7%) across the delivery and recovered to 57.1% (−23.8%) one month after the baby was born. TAPSE stayed within its normal range across the delivery, while TDI-S’ wave velocity deteriorated just after the delivery and did not make a recovery even 3 months after. Although the mother kept good general conditions during the postpartum follow-up for 7 months without presenting any cardiac symptoms, all parameters showed mild deteriorations once again at 7 months after the delivery.
Takeuchi repair was first proposed in 1979 as a physiological repair of ALCAPA that creates an aorto-pulmonary window and an intrapulmonary tunnel using a baffle. Although it has been documented that Takeuchi repair may result in high rates of complications and reoperations mainly due to PR, this intervention is still recommended when a direct reimplantation is deemed difficult, e.g., due to an insufficient length of the anomalous coronary or in the presence of unfavorable coronary anatomy for reimplantation procedure.
The Assessment of Pre-Conceptional Cardiac State
The uniqueness of coronary perfusion after Takeuchi repair, and lack of clinical reports on coronary flow reserve after the operation, make it difficult to assess the cardiac tolerance of the repaired heart during pregnancy and delivery.
In our clinical case, exercise scintigraphy and coronary angiography that took place just one year before the pregnancy ensured that good myocardial blood supply via the Takeuchi route was serving good LV function.
Concerning RV function, the preoperative state was severely impaired in this patient. We decided the surgical intervention based on the recommendation for repaired tetralogy of Fallot.3) A postoperative study revealed successful correction of insufficiency of the pulmonary and tricuspid valves, resulting in RV volume reduction. Our team of cardiologists and obstetricians hence expected that, if followed by careful monitoring and properly treated with analgesia, the woman would have a successful vaginal delivery.
Monitoring and Control during the Pregnant Period
The plasma BNP reaches a peak in early postpartum even in normal pregnancy up to 42.5 pg/mL,4) and in our case, it was elevated to 49.6 pg/mL during the full gestation and decreased to the normal range just after the delivery.
The cardiac ejection fraction calculated by echocardiography does not usually change in healthy women during pregnancy,5) and the chamber size increases slightly reflecting a natural augmentation of the serum volume in this period.
Our data records indicate that the LVEF and the LV size were in the normal ranges during the pregnancy and post-delivery.
An absolute GLS-LV value greater than 20% is likely to be normal according to the recommendations of the American Society of Echocardiography.6) The influence of pregnancy and delivery on the GLS-LV in healthy women remains unclear. Ando wrote that the GLS-LV did not change in pregnancy,7) while Savu described that LV segmental longitudinal systolic deformation is subject to a significant decrease in late pregnancy and reaches again the baseline after 3–6 months of delivery.8) Confirming that trend, GLS-LV values of our case were slightly under the normal range one month before the delivery, and improved after the delivery. Savu also reported that the mean reduction of the GLS-LV at the 3rd trimester was within 10% from the baseline. In that respect, the sequential GLS-LV changes in our case were acceptable as a normal pregnancy.
Concerning LV diastolic function, the E/A ratio was kept over 1.0 and the E/e’ ratio did not change during the pregnancy and the delivery as similarly reported by Díaz9) in normal pregnancy.
When considering the parameter changes of RV function during pregnancy, clinical information is less detailed than that on the LV. Díaz described that RV longitudinal strain was the most relevant parameter for RV function assessments in normal pregnant women, which decreased during gestation probably due to a subclinical dysfunction and afterload changes, followed by improvement after delivery even though these changes were kept in normal ranges.9) In our case, the LS-fwRV value reduction was observed in the late pregnancy and recovered one month after the delivery even that the changes were significantly large, over 50% of baseline.
FAC-RV also deteriorated just after the delivery to 25.4%, apparently impaired value, and recovered to over 50% only one month, while Díaz reported FAC showed a small decline during the normal pregnancy within the normal range.9) We assessed that some degree of RV dysfunction might have occurred during the pregnancy because the patient went through the operation of RVOT reconstruction one year before the delivery.
The sequential change of TDI-S’ wave velocity differs from other parameters, showing deterioration just after the delivery until 7 months later. Díaz observed a similar change of S’ velocity in normal pregnancy and hypothesized that respiratory variations could influence Doppler velocity accuracy.
All parameters of RV function paradoxically showed impaired values 7 months after the delivery. A subclinical RV dysfunction after the surgical operation might have been masked due to the rise in endogenous circulating catecholamines during the pregnancy and delivery, which produced a positive inotropic myocardial response, and then unmasked 7 months later according to the postpartum adaptation.
Kier described that women with pediatric-onset coronary arterial anomalies have a risk of adverse cardiovascular events in pregnancy.10) Kanoh also wrote that symptomatic heart failure might occur during pregnancy in patients with ALCAPA treated through coronary arterial reimplantation when they have persistent myocardial damage.11) These reports underlined the importance of careful assessment and follow-up of patients during and after the pregnancy.
To our best knowledge, Caudwell et al.12) is the only case report in English literature of successful pregnancies and deliveries in two women treated for ALCAPA using Takeuchi repair, though, the hemodynamic parameters and its changes during the pregnancy were not detailed. The successful pregnancy and delivery case reported in this document contributes to the literature on ALCAPA condition treated with Takeuchi repair by presenting the first complete record of sequential cardiac assessments, which confirmed that the good coronary perfusion via the Takeuchi route could support the cardiac stress during gestation.
Our experience also highlighted an important role of RV function in pregnancy as well as good LV function, since the woman got pregnant just after the RV repair regardless of having been infertile for a long term before the last operation. Siemund et al. reported subcritical RV dysfunction associated with impaired uteroplacental circulation in early pregnancy,13) supporting that repair of PR and TR might have improved the fertility in our case. We should probably be engaged in the maintenance of RV function especially for pregnant women with congenital heart disease.
The multidisciplinary expertise of our team was a key element to properly treat the presented maternity. Medical support systems like this are deemed to meet the requirements of an increasing population of adult patients with congenital heart disease.